Hepatitis C is classified among the most dangerous viral infections that have a special propensity to affect liver cells.
After initial infection, the virus invades hepatic tissue and remains silent, while slowly destroying the parenchymal cells of the liver gland. Ironically, most cases of HCV infection are silent and are only instantaneously discovered on routine medical examinations or years after initial infection due to significant alteration in the liver function as a result of virus mediated destruction.
Hepatitis C is considered as life threatening virus and is transmitted by the use of contaminated needles (illicit drug abuse) or accidental needle stick injuries in the hospital setting.
How to Know If You Have Hepatitis C
Since hepatitis infection is mostly asymptomatic, at least in the early course of infection, most people tend to live a normal, symptom-free life. Test for hepatitis C is not generally performed by healthcare providers until the patient is certain of the exposure to a viral source.
There are certain risk factors that are often implicated in the pathogenesis of hepatitis C. If you have one or more of the following risk factors, you should ask your healthcare provider to perform a viral test:
- Your birth year is between 1945-1965.
- You have received a blood transfusion from an unaccredited source or from a donor who is an HCV positive.
- Exposure to contaminated syringes or needles during illicit drug use.
- If you have received blood/ plasma for a blood related disorder or condition especially before 1987.
- If you are a recipient of an organ transplant especially before July 1992.
- You have a history of kidney dialysis in the past.
- You are an HIV positive patient.
- If your mother was infected with HCV at the time of your birth.
If you have any of the risk factors listed above, make sure to speak to your primary care provider to ascertain if you are infected. Doctors usually perform serological test to ascertain if you have an infection and may also perform a liver biopsy taking a tissue sample from your liver to see if the virus has affected the liver tissue significantly.
For more health info and promotions, please follow us on Facebook- Wellness Lab
 |
| Download Wellness Lab Mobile App now for more promotions |
If you like this article, you can share this to your friends and families , together we share the health information and the taste of a healthy life!
































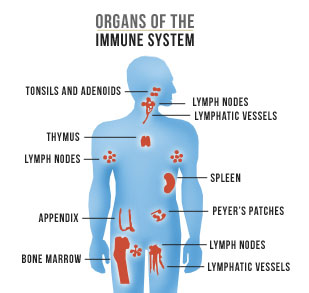 Under normal circumstances, the immune system's white blood cells will protect your body from harmful substances, including viruses, bacteria, cancer cells, and toxins. After the onset of an autoimmune disease, your immune system cripples and fails to differentiate between healthy body tissues and antigens (bacteria, viruses, etc.).This leads to an immune response that destroys healthy body tissues.
Under normal circumstances, the immune system's white blood cells will protect your body from harmful substances, including viruses, bacteria, cancer cells, and toxins. After the onset of an autoimmune disease, your immune system cripples and fails to differentiate between healthy body tissues and antigens (bacteria, viruses, etc.).This leads to an immune response that destroys healthy body tissues.

